“The shift towards VBC models takes deep physician engagement at every step; they need to be involved in the design of the models, the development of the compensation arrangements and the measurement of outcomes. You can’t be successful in a VBC world without the support and engagement of your physicians.”David A. Gregory, Principal, Baker Tilly

Value-Based Care: Physician Engagement
Value-Based Care: Physician Engagement

David A. Gregory
Principal

Michael J. Patti
Principal

Mark Ross
CPA
Partner
The effectiveness of physician’s in your organizations leadership increases the likelihood of implementing a successful value-based contracting (VBC) initiative. Is your organization ready?
To succeed in a VBC environment, healthcare providers need their physicians to be engaged and aligned. That will require more than just financial compensation.
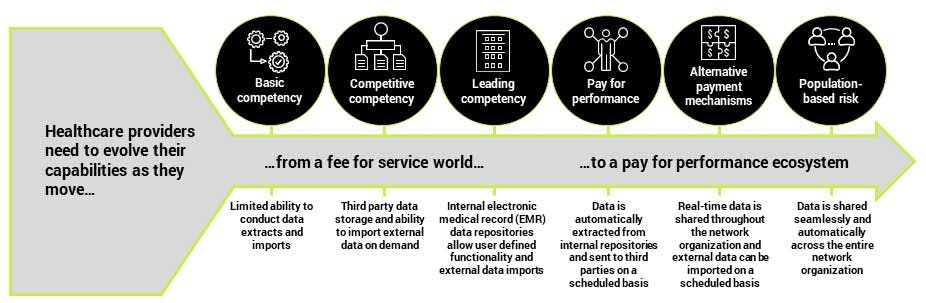
Financial compensation is clearly important – and will remain a key component of the overall physician compensation equation, even in a fully VBC world. Over the coming years, health systems will need to incrementally evolve their compensation models to incorporate a much wider mix of outcome measures.
However, it will take more than just dollars influence physician behavior. For example, physicians can often be motivated by good, insightful data. They tend to be very keen on improving their own operational efficiency. Most of all, they care about delivering good outcomes to their patients.
Five key considerations
- Focus on communication, training and education: Help physicians across the network understand how the shift to VBC models can deliver better outcomes for their patients and themselves. Develop an ongoing communication and training plan that ensures physician capabilities continuously improve as models evolve. Where necessary, provide technology training to those in need.
- Share trusted, insightful data: Physicians need evidence. In addition, they need to trust the data they are seeing, particularly if they are being asked to link their compensation to it. Carefully consider how your organization plans to integrate all of the data – both internal and external – that is needed to measure performance in a VBC world. Furthermore, develop the tools and techniques needed to communicate them in a trusted and comprehensible way.
- Don’t force a single model: Physicians often argue that their specialty is unique. In addition, when it comes to understanding quality and care measures, they are often right. Work closely with each specialty to understand how to engage them and what the most appropriate compensation models and measures might be. Don’t expect to create a one-size-fits-all model for physician compensation in a VBC world.
- Drive evolution through mixed models: If you haven’t done so already, start moving physicians towards a mixed model that combines traditional RVS compensation models with incentives for quality and efficiency outcomes. Avoid simply forcing physicians to put existing compensation “at risk” and focus instead on creating the right mix of incentives to drive the behavior your payers require in a VBC world.
- Involve the docs in decision-making: Whether through regular meetings with physician organizations or joint steering committees and boards, ensure that the physician network is involved, engaged and participating in the decision-making throughout the shift towards VBC models of care.
“Health systems need to think much more holistically about how they engage their physicians – both employed and independent – in the shift to VBC models. Yes, money is important. However, if the physicians don’t feel they had input into the models – or, worse, don’t understand them – you will struggle to fully engage them.”Mary Ellen Kasey, Senior Consultant, Baker Tilly
Two minute self-assessment
Ask yourself whether …
- More than half of your system’s physicians, including those viewed as independents, privileged or contracted, are aligned within an organized entity that spans the entire care delivery spectrum?
- The majority of your physicians are highly engaged in all major strategic initiatives?
- You have well-defined physician participation criteria for VBC programs?
- You have any existing risk-based financial arrangements with physicians or groups?
- The providers in your network and care continuum currently share any financial risk or rewards linked to performance?
If you answered “no” to any of these questions – or if you just don’t know the answer – you may not be ready to assume the risk required to successfully move towards value-based care. Talk to us to find out how you can become ready.
How Baker Tilly can help
Baker Tilly’s team of Value Architects™ provide management consulting, technology and financial planning for healthcare organizations across the health plan, provider and life sciences spectrum.
We have extensive experience helping health systems improve physician engagement and drive the transition to VBC models. From understanding which quality outcomes are important through to setting up, building consensus around and executing new mixed compensation models for physicians, our professionals combine best practice experience, leading technologies and proven approaches to help health systems engage and motivate their physician networks.
Contact us today to find out how Baker Tilly can help your organization.
“Provider and physician leadership must establish new and effective physician compensation models that improve quality and allow for management of the cost of clinical outcomes. Physicians will not buy-in to new care models without a synchronized compensation system, handicapping any move to alternative reimbursement programs.”Michael Patti, Principal, Baker Tilly












