“You can’t expect results from a value-based care contract if your people aren’t able to monitor and manage their performance. Developing the right information sharing capabilities – both technological and strategic – will be key to allowing providers to take on more risk in a pay-for-performance environment.”David A. Gregory, Principal, Baker Tilly

Value-Based Care: Information Sharing
Value-Based Care: Information Sharing

David A. Gregory
Principal

Michael J. Patti
Principal

Mark Ross
CPA
Partner
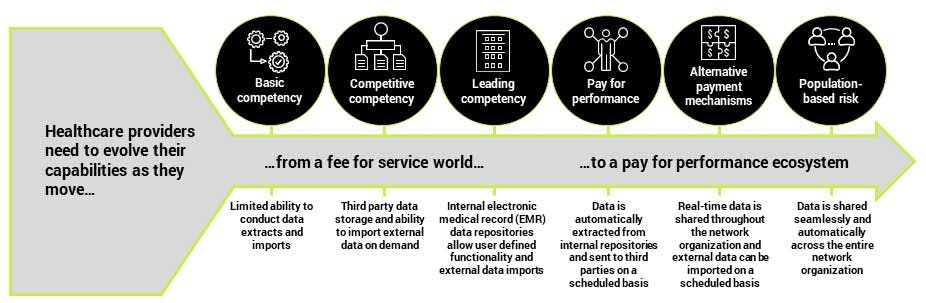
Value-based care (VBC) can help healthcare providers grow their market share and insulate their organizations against some of the downward pressure on fee-for-service reimbursement models. However, embracing and leading in VBC also requires provider organizations to take on increasing levels of risk. Is your organization ready?
In a utopian VBC world, information and data would flow freely between payers, providers, third-party network organizations and patients. Decisions would be based on complete patient information in real time. External data sources such as social determinants of health and population health measures would be continuously integrated into the data stream. Payers and providers would have clear and continuous insight into how they are performing across a wide range of measures.
Today, however, most providers are struggling to share information within their own facilities, let alone with their payers or third-party network providers. Gathering payer data from multiple portals, integrating it with internal and external data sources, and then sharing it across the network organization is an immense challenge.
The shift to VBC may offer providers an opportunity to rethink the way they collect, share and manage data today and in the future.
Five key considerations
- Share the right data: The data that is being shared should align with the incentives that the program objectives are aiming to achieve. Providers will need to work closely with their payers and network organization to identify which data should be shared, and with which players in the care continuum.
- Make it actionable: Carefully consider what types of external data should be integrated to provide key players with insight into both individual patient situations and wider population interventions. Overlay external influences such as social determinants of health and economic data. Integrate data from various payer portals to develop a full picture of population health.
- Go bi-directional: Information must flow up and down the care continuum – from payers down to third parties and back up again. Work with your network organization to standardize data formats and to collaborate on shared systems. Ensure the accountable party has the data they need to achieve their objectives.
- Future-proof it: Recognize that data sources and information requirements will change over time. Build in a level of flexibility to allow for the integration of future measures (such as quality metrics), technologies (like wearables) and objectives. Where possible, lean towards open, cloud-based data architectures and models.
- Explore the technology options: Work closely with your IT function and external consultants to understand the range of technology options available. Identify opportunities to leverage technology to achieve quick wins and rapidly improve data sharing and integration. Collaborate with tech providers to deliver on your vision.
“Information sharing is about enabling your medical professionals to apply the same standard of care and use the same clinical workflows regardless of where their data is coming from. You need to go beyond the traditional one-way transactional data flows that characterized the past and start thinking about data as a shared and integrated resource.”Michael Patti, Principal, Baker Tilly
Two minute self-assessment
Ask yourself whether …
- Your system has a fully functioning electronic medical record (EMR) across all settings of care?
- You have data-mining capabilities and the ability to provide real-time insights to support clinical and business decisions across the population?
- Your IT system is able to aggregate data from various sources, including claims, laboratories, pharmacies and EMRs?
- You have a fully integrated data warehouse, incorporating multiple data types for all care settings (e.g., clinical, financial, demographic, patient experience, participating and non-participating providers)?
- You have data analytics capabilities that enable the evaluation and communication of quality measures within the EMR system?
- You can enable interface, connectivity and data exchange across multiple systems (e.g., acute and non-acute providers, participating and non-participating providers, etc.)?
If you answered “no” to any of these questions – or if you just don’t know the answer – you may not be ready to assume the risk required to successfully move towards value-based care. Talk to us to find out how you can become ready.
“The goal is to make sure the right data is getting to the right person at the right time and at the right cost. Everybody in the population health ecosystem – from payers through to third-party service providers – need to be on the same page and talking the same language. ”David A. Gregory, Principal, Baker Tilly
How Baker Tilly can help
Baker Tilly’s team of Value Architects™ provide management consulting, technology and financial planning for healthcare organizations across the health plan, provider and life sciences spectrum.
From assessing current capabilities and creating strategic road maps for the development of future-ready systems through to identifying and implementing the right technologies and integrating the right data, Baker Tilly’s professionals provide an end-to-end suite of services to help healthcare providers develop and improve their information sharing capabilities.
Contact us today to find out how Baker Tilly can help your organization.
“The complexity of the data challenge can be overwhelming. There are technologies and approaches that can help. But you need to start by taking a step back and thinking strategically about your long-term data strategy and how it drives performance in a value-based care world.”Michael Patti, Principal, Baker Tilly












